Dengue Fever Alert: Prevention, Symptoms & Community Health Tips
In its initial phase, dengue fever frequently mimics other common illnesses, making early detection challenging. The first signs, though nonspecific, act as vital red flags demanding swift medical evaluation. Watch for relentless headaches, muscle and joint discomfort, and an overall sense of malaise. These preliminary symptoms, typically paired with a rapid-onset high fever, must never be dismissed since they can quickly intensify into more dangerous manifestations.
Identifying these early indicators proves essential for prompt treatment and stopping the escalation to graver health issues. When multiple symptoms persist beyond 24-48 hours, consulting a healthcare provider becomes imperative.
Fever and its accompanying symptoms:
A defining feature of dengue is an exceptionally high fever, frequently spiking to 104°F or above. This febrile state usually comes with debilitating headaches, intense bodily pains, and profound weakness. These effects can incapacitate patients and commonly endure for several days. The fever pattern often shows fluctuations, with temperatures rising and falling unpredictably. Tracking these fever variations and associated symptoms proves critical for accurate medical assessment.
Skin Rashes:
A distinctive skin eruption, appearing as either pinpoint red spots or more extensive rashes, may develop as dengue progresses. This dermatological manifestation typically emerges a few days post-fever onset and frequently causes itching. While not universal, its presence serves as an important diagnostic clue, particularly when combined with other telltale signs.
The rash characteristics vary significantly between individuals, making careful observation of skin changes essential. In certain cases, the rash may coincide with abnormal bleeding tendencies.
Severe Dengue Symptoms:
Dengue can sometimes advance to its dangerous form called severe dengue. This critical stage manifests through excruciating abdominal pain, unrelenting vomiting, accelerated breathing, and plummeting blood pressure. These alarming symptoms demand emergency medical care as they may precipitate life-endangering complications.
If you encounter any of these severe manifestations, obtain immediate professional medical assistance. Procrastinating treatment could have dire consequences.
Gastrointestinal Issues:
Digestive disturbances like persistent vomiting and intense abdominal pain often feature prominently in dengue cases. These gastrointestinal problems typically accompany the initial fever and bodily pains, exacerbating the patient's overall distress. While their severity varies, such symptoms always warrant serious attention as possible harbingers of worsening conditions.
Bleeding Tendencies:
Hemorrhagic manifestations including nosebleeds, gum bleeding, or easy bruising may indicate severe dengue progression. These signs appear in certain patients and require urgent medical assessment. Untreated bleeding tendencies risk substantial blood loss and related complications.
Headache and Muscle Pain:
Severe headaches and muscular aches rank among the most commonly reported dengue symptoms. These discomforts typically peak during the illness's initial phase, substantially contributing to patient suffering. While intensity varies, they represent nearly universal features of dengue infection that demand medical attention.
The headache-muscle pain combination, frequently coinciding with fever, can mislead diagnosis, underscoring the need for professional evaluation. Close monitoring enables early intervention and complication prevention.
Preventive Measures for Individuals
Personal Protective Measures
Implementing proactive mosquito bite prevention strategies forms the cornerstone of dengue avoidance. Donning long-sleeved tops and pants during peak mosquito activity hours (dawn and dusk) dramatically reduces exposure risk. Applying EPA-approved repellents containing DEET, picaridin, or lemon eucalyptus oil—following manufacturer guidelines—provides essential protection. Remember to reapply after swimming or heavy perspiration.
Eliminating potential mosquito breeding sites near residences represents another critical preventive step. Regularly empty water-holding containers like plant saucers, bird baths, and rain-collecting vessels. Such elimination efforts substantially reduce local mosquito populations. Promptly repairing leaky plumbing also prevents water accumulation.
Environmental Awareness and Control
Community-based mosquito control initiatives significantly enhance prevention effectiveness. Neighborhood clean-ups targeting standing water sources can drastically cut mosquito numbers. Alerting local health authorities about potential breeding sites facilitates coordinated control measures. This collective approach proves indispensable for community-wide dengue protection.
Maintaining clear drainage systems and unclogged gutters prevents water pooling that mosquitoes require for reproduction. Establishing mosquito-free zones through communal effort represents a proactive dengue prevention strategy. Routine inspections of public areas like parks help maintain safer environments.
Travel Safety Precautions
Travelers to dengue-endemic regions require extra protective measures. Research local mosquito activity patterns and regional risk levels beforehand. Consult physicians about appropriate precautions, including potential prophylactic medications tailored to your itinerary. Heeding local health authority recommendations enhances safety.
Pack protective clothing covering limbs and use recommended repellents. Avoid outdoor activities during peak biting times. Inspect accommodation surroundings for potential breeding sites. Staying informed about regional outbreaks enables smarter travel decisions.
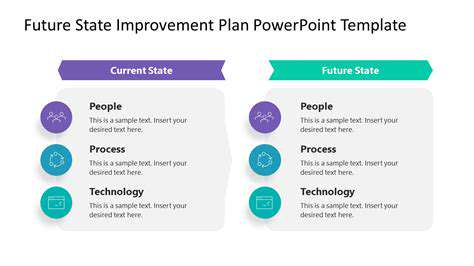
Seeking Early Medical Attention
Recognizing dengue symptoms and obtaining prompt medical care proves vital for effective treatment and complication prevention. Sudden fever, severe headache, muscle/joint pain, or rashes necessitate immediate professional evaluation. Early diagnosis enables proper management and halts disease progression. Understanding early intervention's importance dramatically improves patient outcomes.
Symptom awareness facilitates early dengue detection. Timely medical care prevents disease escalation. Recognizing treatment urgency benefits both individuals and communities. Suspected dengue cases always warrant immediate medical consultation.

Community Health Initiatives and Public Awareness
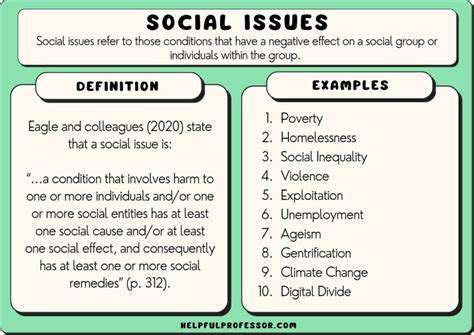
Raising Awareness about Dengue Fever
Dengue fever, a mosquito-borne viral illness, represents a major global health challenge. Effective prevention requires widespread public education campaigns highlighting key symptoms: high fever, severe headache, muscle/joint pain, and distinctive rashes. Early detection enables timely treatment and prevents severe complications.
Community education programs play pivotal roles in dengue prevention knowledge dissemination. These initiatives should detail mosquito life cycles and emphasize eliminating breeding sites like stagnant water near homes. Such knowledge empowers communities to reduce infection risks proactively.
Community-Based Prevention Strategies
Successful community prevention efforts involve residents in identifying and eliminating mosquito breeding locations. Neighborhood clean-up drives effectively decrease mosquito populations. Routine inspections of homes and public areas for standing water, followed by proper disposal or treatment, form crucial strategy components.
Equipping community health workers with appropriate training and resources strengthens prevention networks. These individuals bridge communities and healthcare systems. Training them in symptom recognition, basic first aid, and referral protocols facilitates early intervention.
Vector Control and Mosquito Management
Comprehensive vector control measures are fundamental to dengue prevention. This multifaceted approach surpasses simple insecticide use. Community participation in identifying and eliminating breeding sites—from discarded containers to clogged gutters—proves essential.
Educating residents about proper waste management and environmental hygiene reduces mosquito habitats. Regular public space inspections by officials and volunteers help maintain mosquito-free zones.
Early Diagnosis and Treatment
Prompt dengue diagnosis prevents severe complications and enables effective treatment. Training healthcare providers and community workers in symptom recognition allows early detection. This facilitates timely medical care and reduces severe illness risks.
Accessible, affordable healthcare services including diagnostic tools are vital. Promoting awareness about early medical consultation significantly decreases disease severity.
Public Health Campaigns and Education
Targeted public health initiatives are crucial for dengue awareness. Campaigns should adapt to specific community needs and cultural contexts. Utilizing multiple communication channels—community gatherings, social media, local media—maximizes outreach and impact.
Multilingual educational materials should provide clear prevention information, including personal protection methods like repellent use and proper clothing.
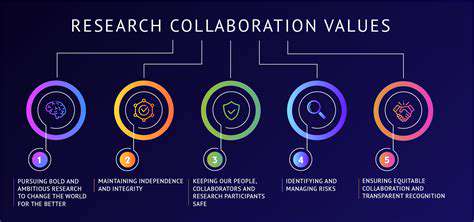
Collaboration and Coordination
Effective dengue control requires robust collaboration among government agencies, community groups, healthcare providers, and individuals. Establishing clear communication channels and coordinated efforts ensures unified responses.
Implementing comprehensive surveillance systems tracking dengue cases enables early outbreak detection and targeted interventions. This data-driven approach facilitates proactive public health measures.